- drsundar@sundarspine.com
- Youtube
For Appointments, Call
+(91) 9080 9680 66
+(91) 9080 9680 66

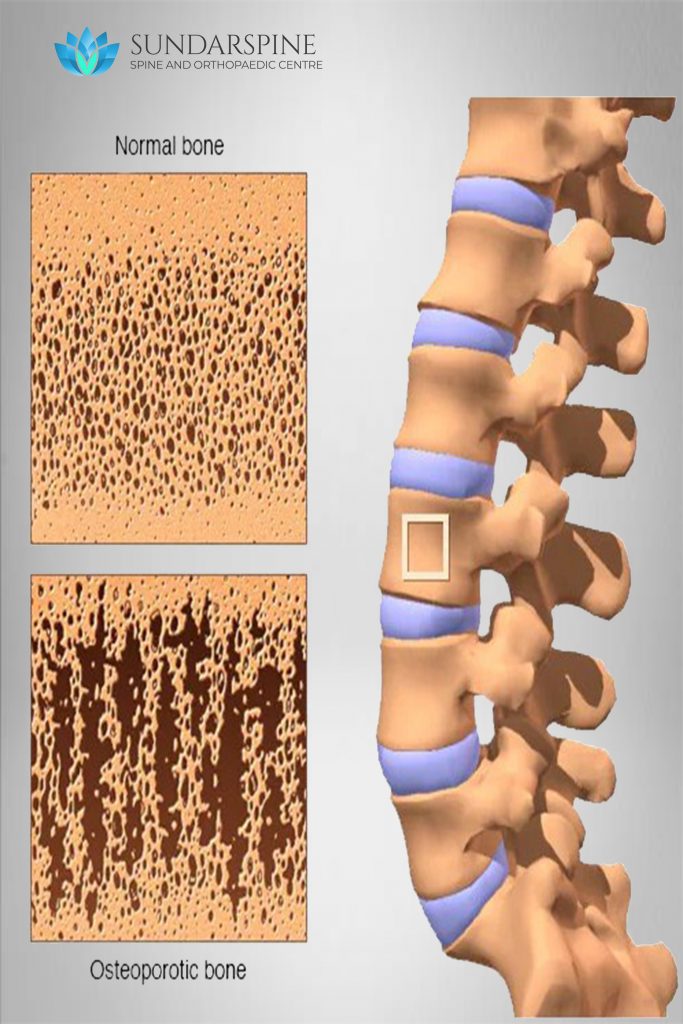
Osteoporosis is a condition that causes bones to become weak and brittle such that a fall or even mild stresses such as bending over or coughing can cause a fracture. Osteoporosis-related fractures most commonly occur in the hip, wrist or spine.
Osteoporosis affects men and women of all races. But white and Asian women, especially older women who are past menopause, are at highest risk. Medications, healthy diet and weight-bearing exercise can help prevent bone loss or strengthen already weak bones.
Symptoms:
Risk factor: Old age, women, post-menopause, thin built, malnourished, family history, post-hysterectomy
Causes:Bone is living tissue that is constantly being broken down and replaced. Osteoporosis occurs when the creation of new bone doesn’t keep up with the loss of old bone.
When to see a Doctor: It you have the above risk factors, periodic follow-up with the doctor is required to detect any change in the bone-mass.
Treatment: Incidental diagnosis can be manages with bone strengthening medications. DEXA scan may be done to assess the bone density. Osteoporotic fracture are treated by case-to-case basis.
Vitamin D deficiency — when the level of vitamin D in your body is too low — can cause your bones to become thin, brittle or misshapen.
Although the amount of vitamin D adults get from their diets is often less than what’s recommended, exposure to sunlight can make up for the difference. For most adults, vitamin D deficiency is not a concern. However, some groups may have lower levels of vitamin D due to their diets, little sun exposure or other factors.
Symptoms:
Children who are deficient in vitamin D can also have muscle weakness or sore and painful muscles. Severe deficiency can cause rickets.
Lack of vitamin D is not quite as obvious in adults. Signs and symptoms might include:
Treatment: Usually Vitamin D and calcium supplement, lifestyle changes, morning walk (at sunrise or sunset time).

Plantar fascitis is one of the most common causes of heel pain. It involves inflammation of a thick band of tissue that runs across the bottom of your foot and connects your heel bone to your toes (plantar fascia).
Symptoms: Plantar fasciitis typically causes a stabbing pain in the bottom of your foot near the heel. The pain is usually the worst with the first few steps after awakening, although it can also be triggered by long periods of standing or when you get up after sitting. The pain is usually worse after exercise, not during it.
Risk factor:
Causes: Your plantar fascia is in the shape of a bowstring, supporting the arch of your foot and absorbing shock when you walk. If tension and stress on this bowstring become too great, small tears can occur in the fascia. Repeated stretching and tearing can irritate or inflame the fascia, although the cause remains unclear in many cases of plantar fasciitis.
When to see a Doctor: Consult a doctor when the pain is unbearable, affecting your day-to-day routine.
Treatment: Initially managed by medication and plantar stretching exercises. Steroid injection can be advised for chronic pain.

Tennis elbow (lateral epicondylitis) is a painful condition that occurs when tendons in your elbow are overloaded, usually by repetitive motions of the wrist and arm.
Despite its name, athletes aren’t the only people who develop tennis elbow. People whose jobs feature the types of motions that can lead to tennis elbow include plumbers, painters, carpenters and butchers.
The pain of tennis elbow occurs primarily where the tendons of your forearm muscles attach to a bony bump on the outside of your elbow. Pain can also spread into your forearm and wrist.
Symptoms:
Treatment: Mild symptoms may be treated by medications and stretching exercise. Restriction in activity. Severe chronic symptoms may have relief with steroid injection.
